
The Future is Hybrid
Because of the pandemic, telemedicine went from a practice optional fridge benefit, to a must have. The pandemic *appears* to be waning for the time being, so what does this mean for digital healthcare, considering the explosion of telemedicine and digital appointments we saw in ’20 and ’21 ? Physical (in-office or in-person) doctor/patient encounters still matter and are essential for the some patient needs and experiences. Because of this we conclude that the near future of healthcare lies in a hybrid-care model. In this model, in-person care is combined with virtual and digital elements, such as telehealth visits and remote patient monitoring (RPM). The key to success for a practice is finding the right blend of in-person and digital services.
The following are areas where you can focus to create a hybrid-care strategy for your practice.
Patient Education
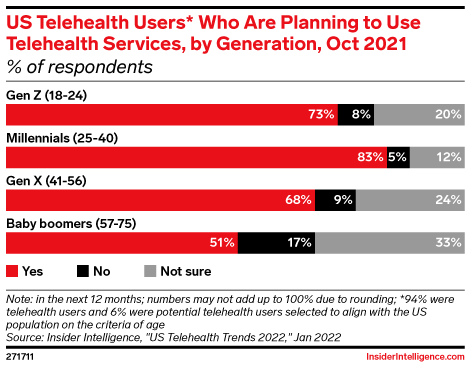
With this increased adoption of telehealth, healthcare organizations must continue to educate consumers on the benefits of virtual care. A large part of the challenge lies in educating the older generations about the benefits.
To help accomplish this aspect, a clear and concise messaging system and strategy, contained within a comprehensive platform, will allow your practice to better educate your patients. By streamlining and optimizing your digital healthcare outward communitive solutions, bolsters your practice’s ability to educate existing, new, and potential patients on hybrid practice offerings. A streamlined solution also allows for all forms and methods of communication between practice and patient or between lab and practice. Closing these communication gaps can lead to well-rounded customer education, lower no-show rates, as well as improved practice reach and practice reputation.
Telemedicine & Virtual Visits Expansion
A cohesive telehealth strategy has become a must for successful practices. Telehealth is an essential inclusion of hybrid patient-centered care. Furthermore, a successful strategy requires identifying and executing the right mix of in-person, virtual visits, and telehealth offerings. By using and expanding telehealth in the right setting, physicians can provide proactive care, lower costs, and can help providers improve their services by reducing the need for regular in-person visits. The combination of these two types of care also helps physicians provide more individualized care, which is another key factor in patient outcomes and practice success.
Furthermore, when practices expand telemedicine and virtual visits patients can rely on a certain level of personal risk avoidance. Avoiding risks such as time associated with antiquated laboratory testing and results distribution. By leveraging virtual visits and telehealth, patients can receive quicker and more adequate education on their lab results, through their preferred channel of communication.

Closing the workflow gaps
A hybrid approach cannot flourish without integration and interoperability. Telemedicine, in-office appointments, EHR, and other virtual care offerings all must be integrated for smooth and effective patient experience and practice operations. Practice workflow interoperability is not just about sharing information; it involves the accurate management of data and complex context(s) across different systems. It is essential to ensure that healthcare organizations share health records from multiple sources, so that clinical research teams can access patient and physician data and manage care. However, achieving this requires a careful assessment of the practice’s current state of system interoperability. Without a robust hosting platform, such as VOLA, these gaps can cause digital bottlenecks, which causes frustrations and inefficient care.
By implementing these interoperability features, health organizations can stop treating individuals as a health plan member and start treating them as patients. They will also be able to better protect patient information by ensuring that the infrastructure is secure and the entities verify authorization. By leveraging an interconnected system, healthcare decision-makers will be able to better understand their patients’ needs and ultimately improve their delivery of hybrid care.
Expansion of RPM
In addition to telemedicine, a hybrid practice must utilize a variety of methods to remotely reach patients. One of these methods is the RPM (Remote Patient Monitoring). Remote Patient Monitoring (RPM) technology enables doctors to monitor patients from anywhere. Furthermore, RPM technology has developed to the extent that the patient can be allowed normal daily activities at home while still being monitored with the use of modern communication and wearable sensor technologies. Sensors for monitoring essential vital signs such as electrocardiogram reading, respiration rate, heart rate, temperature, blood glucose levels, blood pressure, and even brain activity, just to name a few.
For RPM to work, the communication and accompanying infrastructures must be concise, connected at all times, and be accessible through multiple communication channels (for the patient and provider). When this RPM optimization is achieved, it opens the door for a robust care plan including anything from initial patient educational services to illness prevention. RPM, when implemented correctly, allows you to reach more patients, improve quality of healthcare, and ultimately, improve patient outcomes.
Going Hybrid
It’s clear, for the time being, in-office patient visits are not going away. This fact, as well as the rapid emergence of telemedicine and virtual health offerings are leading to a new hybrid care delivery model. To thrive in this evolving space, practices must use cohesive and comprehensive technology platforms to create long-term strategy and actual workflows for hybrid healthcare delivery. While hybrid is an excellent option, your practices’ implementation strategy needs to be well-designed and effective. Executing this implementation correctly means your hybrid healthcare system can have a high rate of success.
In closing, with a successful hybrid approach, healthcare professionals can gain a more comprehensive understanding of a patient’s health condition at any time from anywhere, which can lead to more accurate diagnoses and medication prescribing, fewer emergency room visits, and more time between in-office visits. Which no doubt produces better patient outcomes and helps to remedy an extremely strained healthcare system.
Interested in a demo to see our platform can be optimized for your organization hybrid aspirations? Schedule a demo with the VOLA team today! Contact Us.
About VOLA
Our mission is to support the rapidly growing digital transformation of the healthcare industry. We do this by equipping medical offices and telehealth providers with customizable and affordable technology. One of our key differentiators is our ability to connect laboratory tests into the workflow of telehealth services. Additionally, we have a dedicated SaaS product line to support laboratories and laboratory marketing organizations.

